Connect With Us
Blogs

Do Your Feet Grow During Pregnancy?

Pregnancy affects nearly every part of the body, including your feet. Many pregnant women notice their feet changing in size. Studies show increases in length, width and volume during pregnancy. This is often due to hormonal changes that loosen ligaments and cause arches to flatten. Fluid retention can also lead to swelling, making shoes feel tighter or uncomfortable. Symptoms may include aching arches, increased shoe size, swollen ankles, and a general feeling of heaviness or fatigue in the feet, especially later in pregnancy. A podiatrist can provide significant relief during this time. They offer custom orthotics to support fallen arches, advice on proper footwear, and treatment to reduce swelling and pain. Routine care from a podiatrist can prevent long-term foot issues and help maintain mobility and comfort throughout pregnancy. If you are dealing with this condition, it is suggested that you make an appointment with a podiatrist.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with Steven Black, DPM from California . Our doctor will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Pregnancy and Foot Health
Many pregnant women complain about foot pain while they are expecting. Foot pain can primarily be caused by weight gain and hormonal changes taking place in the body. By understanding how pregnancy impacts the health of a woman's feet, a pregnant woman can take action to keep her feet as healthy and comfortable as possible.
Because a woman's weight changes during pregnancy, more pressure is brought to bear on both the legs and the feet. This weight shift can cause two major foot problems: over-pronation, also known as flat feet, as well as edema, which is swelling of the feet. Over-pronation occurs when the arch of the foot flattens, causing the foot to roll inwards when the individual is walking, and can aggravate the plantar fascia tissues located along the bottom of the feet. If these tissues become inflamed, a pregnant woman can experience pain in the heel of the foot as well as severe foot pain while walking or standing. Swelling of the feet, or edema, often occurs in the later stages of pregnancy. It is caused by slow circulation and water retention, and may turn the feet a light purple color.
To keep feet in good health and prevent over-pronation, pregnant women should avoid walking barefoot and be sure they are wearing shoes that offer good arch support. A device known as an orthotic can be added to regular footwear in order to provide additional support for the feet during pregnancy. Any expectant mother whose feet hurt should first check to see if the shoes she is wearing are old, worn out and not offering the proper support necessary for distributing the weight of her body during pregnancy.
To treat edema of the feet, a good start is to wear quality footwear which offers support and good circulation. Keep feet elevated whenever possible by using a foot stool while seated. Stay well hydrated by drinking plenty of water to prevent water retention in the feet. Any swelling that occurs in only one foot should be examined as soon as possible by a doctor.
Good foot health during pregnancy can help expectant mothers avoid foot pain that leads to other health problems. Massaging the feet and doing regular gentle exercise like walking aids foot health by contributing to good circulation. Supportive shoes are also a good investment that will support foot health during pregnancy.
Identifying a Toe Fracture

A toe fracture is a break in one of the small bones of the toe, often caused by trauma such as stubbing the toe, dropping something heavy on it, or sports injuries. Symptoms include pain, swelling, bruising, and difficulty walking. The affected toe may appear crooked or misaligned. Diagnosis typically involves a physical examination and imaging tests like X-rays to confirm the extent and location of the break. A podiatrist can assess the injury and recommend appropriate care, which may include splinting, protective footwear, or, in some cases, surgery. If you suspect a broken toe, it is suggested that you visit a podiatrist promptly to ensure proper healing and to avoid long-term complications.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Steven Black, DPM from California . Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
Spotting a Foot Stress Fracture

A foot stress fracture is a small crack in the bone caused by repetitive stress rather than a single traumatic event. It often develops over time and is common among athletes and individuals who suddenly increase their activity level. Risk factors include wearing poor footwear, weakened bones, and high-impact sports. Causes may involve overuse, improper training, or biomechanical issues. Symptoms include localized pain, swelling, tenderness, and discomfort during activity. A podiatrist can confirm the diagnosis through imaging tests, recommend rest, footwear changes, and possibly immobilization to ensure proper healing. If you have persistent foot pain that worsens with activity, it is suggested that you promptly schedule a visit with a podiatrist to receive expert care and prevent complications.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Steven Black, DPM from California . Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
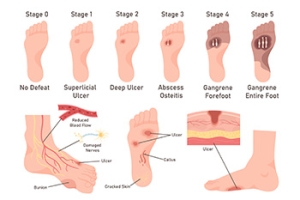
Managing Diabetic Foot Ulcers
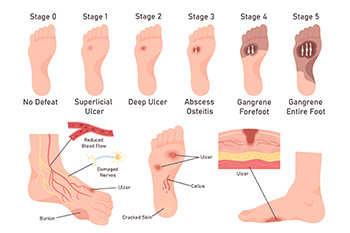
Diabetic foot ulcers are open sores or wounds that commonly occur on the bottom of the foot in people with diabetes. They are caused by poor circulation, nerve damage or neuropathy, high blood sugar levels, and repetitive pressure or trauma to the feet. Because nerve damage can dull pain sensations, many patients may not feel the ulcer forming until it becomes severe. Symptoms include redness, swelling, drainage, or a foul odor. The area may feel warm, and in some cases, there can be pain, although many feel little to none due to neuropathy. Untreated ulcers can lead to serious infections or even loss of limb. A podiatrist plays a key role in managing diabetic foot ulcers by offering treatments like offloading that reduce the pressure on the wound, wound debridement to remove dead tissue, specialized dressings, and infection control. Custom orthotics or diabetic shoes may also be recommended. If you have diabetes and have a foot ulcer, it is suggested that you are under the care of a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Steven Black, DPM from California . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
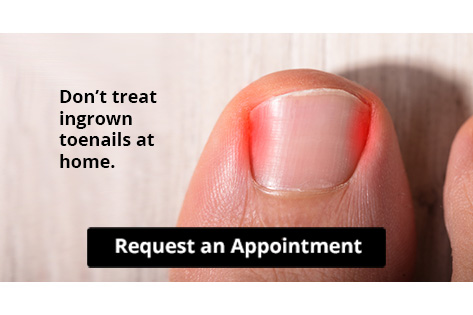
Let the Expert Treat Your Ingrown Toenails
Painful Ingrown Toenails

Ingrown toenails occur when the edge of the toenail grows into the surrounding skin, often affecting the big toe. This common condition can be caused by trimming toenails too short, wearing tight shoes, injury, or a natural curve in the nail. Symptoms include redness, swelling, pain along the nail edge, and sometimes drainage or infection, if left untreated. The area may feel tender to the touch and become increasingly painful when walking or wearing shoes. A podiatrist can diagnose an ingrown toenail with a simple exam. Treatment may involve gently lifting the nail edge, removing a portion of the nail, or prescribing antibiotics if an infection is present. In recurring cases, a minor procedure can permanently remove part of the nail to prevent future problems. Proper nail care and footwear recommendations can also help prevent recurrence. If you have developed an ingrown toenail, it is suggested that you promptly schedule an appointment with a podiatrist who can effectively treat this condition.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Steven Black, DPM of California . Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.