Bunions, also called hallux valgus, develop when the big toe drifts toward the second toe and the joint at its base sticks out. The primary risk factor for bunions is inherited foot structure, particularly a misaligned metatarsophalangeal, or MTP joint. People with flat feet, excessive pronation, or loose-joint mobility place uneven pressure across the forefoot, increasing the likelihood of progression. Arthritis, prior foot injuries, and certain neuromuscular conditions can also weaken joint stability and contribute to deformity. Although tight or high-heeled shoes do not directly cause bunions, they commonly aggravate symptoms and speed irritation in people already predisposed. A podiatrist evaluates alignment, orders imaging, and provides medical treatment options to reduce pain, limit deformity progression, and improve walking function. If you have foot problems associated with bunions, it is suggested that you make an appointment with a podiatrist for an exam, diagnosis, and ongoing treatment.
If you are suffering from bunions, contact Steven Black, DPM of California . Our doctor can provide the care you need to keep you pain-free and on your feet.
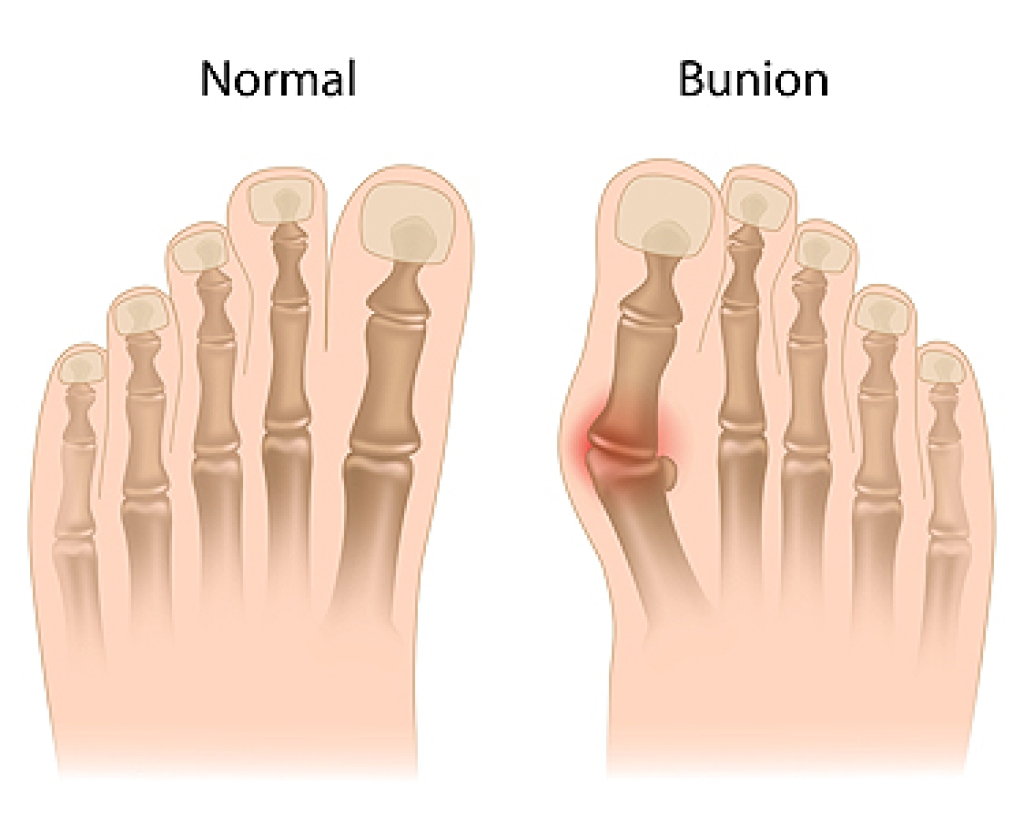
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Podiatrists often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your provider.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.