
Orthotics, specialized shoe inserts designed to support and align the foot and ankle, are crafted by a myriad of companies worldwide. However, amidst this diversity, podiatrists stand out as experts in the field. These healthcare professionals possess extensive knowledge of foot anatomy, biomechanics, and gait analysis, enabling them to tailor orthotic solutions to individual needs effectively. Unlike mass-produced inserts, podiatrists meticulously assess each patient's unique requirements, accounting for factors like foot structure, medical history, and lifestyle. This personalized approach ensures optimal fit and function, addressing a wide range of conditions, from plantar fasciitis to diabetic foot complications. Podiatrists employ a variety of techniques and materials, including foam impressions, computerized scans, and custom molds to create orthotics that provide maximum comfort and support. Furthermore, they offer ongoing care and adjustments, ensuring patients experience lasting relief and improved mobility. If you experience foot or ankle discomfort, it is suggested that you schedule an appointment with a podiatrist to discuss whether custom-made orthotics can help you.
If you are having discomfort in your feet and would like to try orthotics, contact Steven Black, DPM from California . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
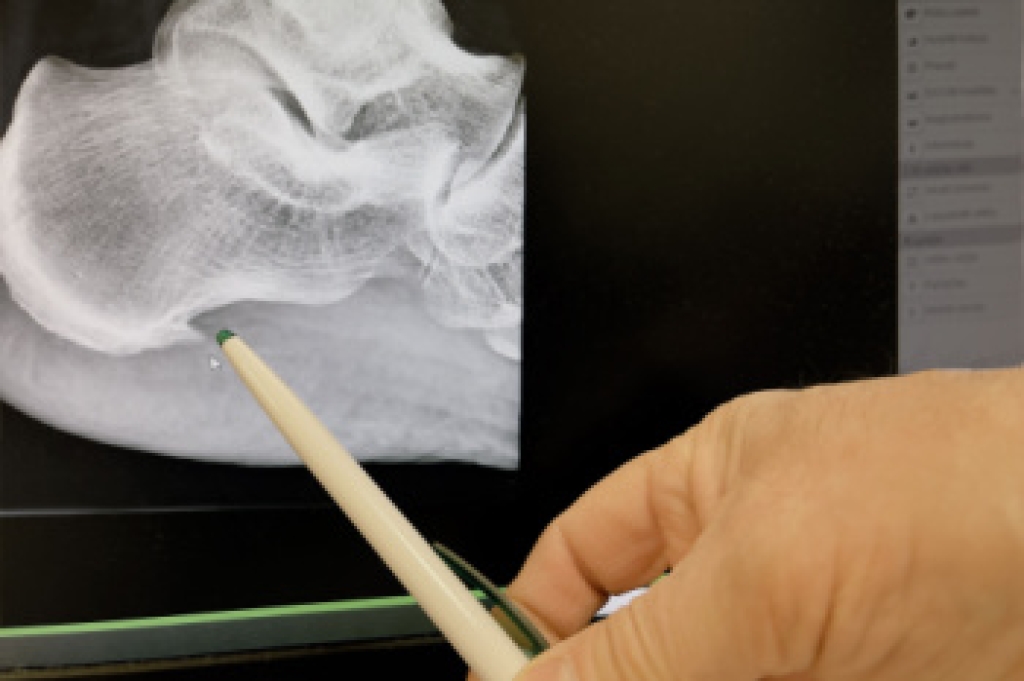
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.






 Flatfoot
Flatfoot