Connect With Us
Blog

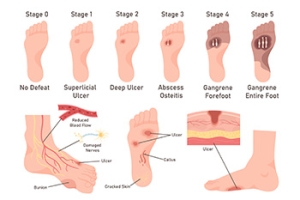
Managing Diabetic Foot Ulcers
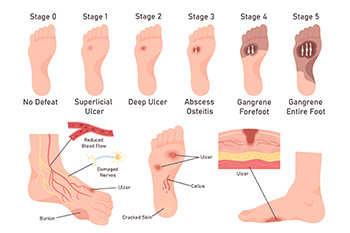
Diabetic foot ulcers are open sores or wounds that commonly occur on the bottom of the foot in people with diabetes. They are caused by poor circulation, nerve damage or neuropathy, high blood sugar levels, and repetitive pressure or trauma to the feet. Because nerve damage can dull pain sensations, many patients may not feel the ulcer forming until it becomes severe. Symptoms include redness, swelling, drainage, or a foul odor. The area may feel warm, and in some cases, there can be pain, although many feel little to none due to neuropathy. Untreated ulcers can lead to serious infections or even loss of limb. A podiatrist plays a key role in managing diabetic foot ulcers by offering treatments like offloading that reduce the pressure on the wound, wound debridement to remove dead tissue, specialized dressings, and infection control. Custom orthotics or diabetic shoes may also be recommended. If you have diabetes and have a foot ulcer, it is suggested that you are under the care of a podiatrist.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Steven Black, DPM from California . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
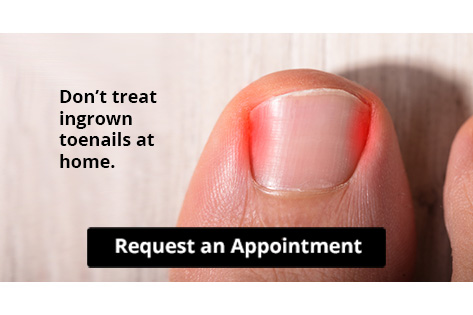
Let the Expert Treat Your Ingrown Toenails
Painful Ingrown Toenails

Ingrown toenails occur when the edge of the toenail grows into the surrounding skin, often affecting the big toe. This common condition can be caused by trimming toenails too short, wearing tight shoes, injury, or a natural curve in the nail. Symptoms include redness, swelling, pain along the nail edge, and sometimes drainage or infection, if left untreated. The area may feel tender to the touch and become increasingly painful when walking or wearing shoes. A podiatrist can diagnose an ingrown toenail with a simple exam. Treatment may involve gently lifting the nail edge, removing a portion of the nail, or prescribing antibiotics if an infection is present. In recurring cases, a minor procedure can permanently remove part of the nail to prevent future problems. Proper nail care and footwear recommendations can also help prevent recurrence. If you have developed an ingrown toenail, it is suggested that you promptly schedule an appointment with a podiatrist who can effectively treat this condition.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Steven Black, DPM of California . Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenail Care
An ingrown toenail is a toenail that grows sideways into the nail bed, causing pain and swelling. Ingrown toenails can worsen and cause drainage, turning into a serious infection.
Several factors affect whether a person is at risk from an ingrown toenail. The many causes include being overweight, diabetes, participating in sports, having a fungal infection of the toe, and cutting your nails too short. Ingrown toenails also have a genetic predisposition, causing some people to be more prone to receive the condition than others. Other causes include improperly fitting shoes and shoes that keep the feet damp.
Ingrown toenails can be preventable with certain measures. For starters, allowing your toe nails to grow slightly longer in length will help prevent them from becoming ingrown. If you have already developed an ingrown toenail, soak the affected toe in warm water. This will alleviate the pain and help prevent an infection from forming. Antibiotic soap or Epsom salts may be added to further help the relieving process and avoid infection. Placing cotton beneath the affected area is also suggested, as this may help the toenail grow upwards and not into the nail bed. Swelling and redness can be reduced by resting with your feet elevated.
A podiatrist should be seen if the pain becomes so serious that it prevents you from doing your everyday activities. If a red streak running up your leg appears or if you suspect your infection has spread, contact a podiatrist immediately. Fast treatments can be undertaken to lessen your pain and have you walking comfortably.
An ingrown toenail can be easily treated with a Band-Aid. Simply wrap the affected toe with a Band-Aid to prevent infection and keep the nail from growing out at a painful angle.
In more serious cases, your podiatrist may decide to make a small incision to remove a portion of your toenail. To prevent the nail from growing back, medication will be placed directly into the nail bed. This procedure would be performed under local anesthesia and is a faster method to alleviate discomfort from an ingrown toenail. Post-procedure directions will have you stay off the affected foot for a day. Afterwards, normal activities can be resumed.
Options for Ingrown Toenail Surgery

Ingrown toenails develop when the edge of the nail grows into the surrounding skin, leading to pain, redness, swelling, and sometimes infection. Causes include improper nail trimming, tight shoes, toe injuries, or naturally curved nails. The area may feel sore, swollen, and, in more severe cases, may produce drainage or pus. When conservative treatments like warm soaks, antibiotics, or lifting the nail fail, a podiatrist may recommend a minor surgical procedure. One common option is partial nail avulsion, where only the ingrown portion is removed. Another method is a wedge resection, where the side of the nail and a portion of the nail bed are removed to stop the problematic section from growing back. These in-office procedures are quick, performed under local anesthesia, and typically offer long-term relief. If you have a painful ingrown toenail, it is suggested that you schedule an appointment with a podiatrist who can determine if surgery is right for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Steven Black, DPM of California . Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
When Steroid Injections May Help Foot and Ankle Pain

Foot and ankle disorders, such as plantar fasciitis, arthritis, bursitis, and tendonitis, can cause persistent pain and inflammation that interferes with daily life. When rest, targeted exercises, and oral medications are not enough to bring relief, a podiatrist may recommend a steroid injection. These injections contain corticosteroids, which are anti-inflammatory medications delivered directly into the affected area to reduce swelling and ease discomfort. In many cases, they offer temporary but significant relief and allow patients to continue with rehabilitation or maintain mobility. Injections are often used in conjunction with other treatments, such as custom orthotics or stretching routines. Although generally safe, repeated use of steroids in the same area should be carefully monitored to avoid tissue damage. If your foot or ankle pain has not improved with other, more conservative care, it is suggested that you speak with a podiatrist about whether a steroid injection may be appropriate for your condition.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Steven Black, DPM from California . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
What Is Charcot-Marie-Tooth Disease?
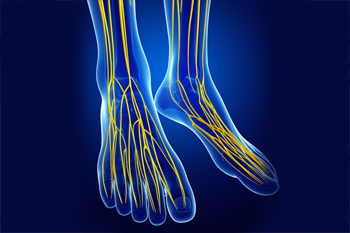
Charcot-Marie-Tooth disease is a rare inherited disorder that affects the peripheral nerves, which are responsible for controlling muscles and relaying sensory information. This condition gradually damages the nerves, often leading to muscle weakness and decreased sensation in the feet and lower legs. People with Charcot-Marie-Tooth may develop high arches, curled toes, and an abnormal gait due to the weakening of foot and leg muscles. Over time, the condition can result in balance issues, foot deformities, and difficulty walking. Symptoms often begin in childhood or early adulthood and typically progress slowly. While there is no cure, treatment options like custom orthotics and supportive footwear can help manage discomfort and improve mobility for those living with this lifelong condition. If you have this condition, it is suggested that you are under the care of a podiatrist who can help you to manage Charcot-Marie-Tooth disease.
Some foot conditions may require additional professional care. If you have any concerns, contact Steven Black, DPM of California . Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Blog Archives
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022