Connect With Us
Blog

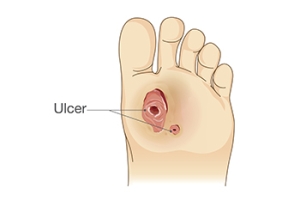
Causes and Treatment of Foot Ulcers
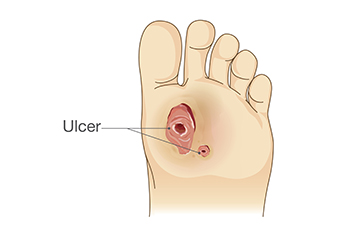
Foot ulcers are open sores or wounds that typically develop on the bottom of the foot and can result from poor circulation or prolonged pressure. They are often linked to conditions like peripheral neuropathy, arthritis, and Raynaud's phenomenon. Peripheral neuropathy reduces sensation in the feet, making it difficult to detect injuries, while poor circulation from conditions like Raynaud's delays healing. Arthritis can increase the risk of pressure ulcers by altering foot mechanics. If untreated, foot ulcers can lead to severe infections, including gangrene, possibly resulting in amputation. Symptoms include swelling, redness, drainage, and pain surrounding the wound. Diagnosis involves physical examination and tests to assess circulation and nerve function. Treatment includes wound care, offloading pressure, managing underlying conditions, and sometimes surgery. Healing time varies, from weeks to months, depending on the ulcer's severity and the patient's overall health. If you have developed a foot ulcer, it is strongly suggested that you schedule an appointment with a podiatrist for treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Steven Black, DPM from California . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Practical Tips for Senior Fall Prevention

Falls among seniors are a significant concern, often resulting from a combination of factors. Common causes include muscle weakness, poor balance, vision problems, and environmental hazards like clutter or uneven floors. Medication side effects and medical conditions such as arthritis can also contribute to fall risk. To prevent falls, it is important to implement several practical strategies. Ensure the home environment is safe by removing trip hazards, installing grab bars, and improving lighting. Encourage regular exercise to enhance strength and balance like walking or specialized fall prevention classes. Regular eye exams and reviewing medications can also help address underlying issues. If you have injured your foot or ankle from falling, it is suggested that you consult a podiatrist who can treat various conditions.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Steven Black, DPM from California . Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
The Healing of a Broken Foot

A broken foot occurs when one or more of the bones in the foot are fractured, often due to trauma, such as a fall, car accident, or sports injury. Symptoms typically include intense pain, swelling, bruising, and difficulty walking or bearing weight. The severity of the fracture, its location, and the treatment approach all influence healing time. Generally, a simple fracture can take six to eight weeks to heal, while more complex fractures may require several months, especially if surgery is needed. During the healing process, immobilization with a cast or boot is usually prescribed, and in some cases, crutches are provided to avoid putting weight on the foot. If you have broken your foot, it is suggested that you schedule an appointment with a podiatrist and follow their instructions to ensure proper healing and avoid complications.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Steven Black, DPM from California . Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Get Professional Care for a Broken Foot or Ankle
Features of Running and Walking Shoes

Running shoes and walking shoes are designed with distinct features tailored to their respective activities. Running shoes are built to handle the higher impact forces of running, featuring more cushioning in the heel to absorb shock and provide support during each stride. They often have a more pronounced heel-to-toe drop, which promotes a forward motion. In contrast, walking shoes are designed for lower impact and typically have a flatter sole, offering even cushioning and greater flexibility. The emphasis in walking shoes is on stability and comfort for the repetitive heel-to-toe motion of walking. Additionally, walking shoes usually have a more rigid midsole to support the arch and enhance stability. Choosing the appropriate shoe based on your activity helps prevent injury and ensures better performance and comfort. If you have endured a foot or ankle injury from wearing the wrong type of shoes, it is suggested that you consult a podiatrist who can treat various foot conditions, and guide you on which shoes to buy for your desired activity.
For more information about walking shoes versus running shoes, consult with Steven Black, DPM from California . Our doctor can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Differences between Walking and Running Shoes
Both running and walking are great exercises, but should a person wear the same shoes for both activities? The answer is no, because there is a difference between the way a person’s feet hit the ground when they are walking and when they are running. Therefore, the shoes for each activity are designed differently. Before you begin any exercise program it is always recommended that you speak with your doctor or podiatrist.
Walking is a low impact exercise that is often recommended by doctors to their patients. While walking is a simple activity, it still requires some degree of preparation. If you think about walking and how your feet strike the ground as you move, you will notice that your heel hits the ground first before your foot continues to roll forward and your next step begins. Because of this rolling motion, walking shoes are designed to be more flexible than running shoes. This flexibility helps the walker push off with each step taken.
Because the heel hits the ground first when you walk, walking shoes are designed to absorb most of the shock. Walking shoes should therefore have a beveled or angled heel. The angle of the heel helps absorb the shock and reduces pressure from the ankles. This is especially important for speed walkers, as their feet will hit the ground twice as often as the normal walker.
When people decide to run as a hobby or for their health, they must first realize that running is a high impact exercise. If not done with the proper equipment, running may cause damage to the feet and legs. Running shoes are designed to be more lightweight and to have thicker soles. The thicker soles act as shock absorbers for the rest of the body. Walking shoes often do not have the proper arch support that running shoes do.
A proper fitting shoe can make or break a runner or a walker. If the shoes are too big, their feet will slide back and forth inside the shoe and cause blisters. Whether you will be running or walking, the right equipment can make all of the difference in the world.
Plantar Fasciitis Stretches

Plantar fasciitis is a common cause of heel pain, primarily resulting from inflammation of the plantar fascia, the thick band of tissue running along the bottom of the foot. Common causes can include excessive stress from high-impact activities, prolonged standing, wearing unsupportive footwear, or being overweight. Symptoms typically include a sharp, stabbing pain in the heel, especially noticeable with the first steps in the morning or after prolonged periods of rest. Treatment focuses on reducing inflammation and relieving pain. Effective stretches include the calf stretch, where you press against a wall with one leg forward and the other extended back. Another is the plantar fascia stretch, where you pull your toes toward your shin while seated. Wearing supportive shoes or custom orthotics, in addition to performing these stretches, can provide significant relief. If you are experiencing symptoms of plantar fasciitis, it is suggested you schedule an appointment with a podiatrist for expert care to effectively manage your condition and improve your foot health.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Steven Black, DPM from California . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Lancaster, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022